Clinical Studies
Transmission of disease in dogs by toothbrushing
- Richard T. Glass, DDS, Ph.D.
- Mary E. Martin, RDH, DDS**
- Larry J. Peter, DVM, MS***
Introduction
In 1986 a systematic study was published concerning microorganism
found on the toothbrushes of "healthy" dental patients and patients
with inflammatory disease, and as controls, toothbrush out of the
packages1. As expected, the microorganism that grew from
the inflammatory disease patients were those known to produce local
(dental) or systemic diseases. Pathogenic microorganism were also
found on toothbrushes from "healthy" patients. Of equal concern was
that four of five toothbrushes from on manufacturer were
contaminated in the package.
After the initial study, experiments
were performed either the delineate the problems of the toothbrush
further or the find some means of decontaminating the toothbrush.
When known quantities of herpes simplex virus type 1 (HSV-1) were
introduced to sterile toothbrushes, it was found that substantial
numbers of the virus could be retrieved after 48 hours from
artificially dried toothbrushes (HSV-1 is usually killed by
drying)2. If the toothbrush were maintained in a moist
environment (similar to that of a bathroom), almost one half of
original number of virus could be retrieved after seven days. Vital
staining of the microorganism reveals a propensity of the
microorganism to adhere to defects in the bristles (both shaft and
ends) and the cores of natural bristle brushes. These positions of
adherence often were associated with proximate jagged bristle edges.
Thus, two of the necessary criteria for transmission of disease were
met: (1) presence of the microorganism and (2) a potential portal of
entry.
The attempts at toothbrush decontamination were less
fruitful than those of delineating the problem of the toothbrush.
Chemical disinfectants had difficulty in penetrating the aggregates
of microorganism and penetrating the toothbrush bristle depth and
defects. Microwave disinfecting was hampered by the arcing of the
metal cleats used to anchor the toothbrush bristles. Disinfecting
could be achieved using the microwave; however, the resultant
distorted and convoluted toothbrush was not functional. Ultraviolet
light disinfecting is promising in killing microorganisms by needs
further investigation.
Although the data from patients implicated
the toothbrush as a harborer of microorganism, and although the in
vitro studies gave further insight, the final step that was
necessary in deciding the importance of these findings was to have a
controlled environment in which to study actual disease
transmission. Dogs were chosen for a number of reasons, including
the ease which their teeth could be brushed. The following study was
conducted to answer these questions:
1. Does tooth and gingival
brushing with a sterile toothbrush produce gingival brushing
with
or oral other lesions?
2. Does tooth and gingival brushing with a reused,
self-contaminated toothbrush
produce more gingival or other oral
lesions than does brushing with a sterile
toothbrush?
3. Does tooth and gingival brushing with a toothbrush contaminated with106 microorganism(Bacteroides melaninogenicus, Staphylococcus aureus, or Candida albicans) produce more gingival or other oral lesions than does brushing with a sterile or a reused self-contaminated toothbrush? Do these lesions contain the target microorganisms? Can the target microorganisms be recovered from the venous blood within 30 minutes after initial brushing and the gingiva or gingival lesions 24 hours after initial brushing?
4. Does either frequency of tooth and gingival brushing or immune status of the subject alter the incidence of oral or gingival lesions?
Methods and materials
Eighteen healthy adults dogs were used in the study after a
ten-day quarantine. Baseline gingival and venous blood cultures were
made at the beginning of the study. The dogs were equally into three
groups to answer questions 1, 2, and 3.
Dogs in group 1 had their
teeth and gingiva brushed with a new initial sterile on Monday,
Wednesday, and Friday for the first month of the study. Dogs in
Group 11 had brushed their teeth and gingiva brushed with a
initially sterile, but subsequently reused, toothbrush on Monday,
Wednesday, and Friday for the first month of the study. The
toothbrushes used on dogs in group 11 were stored between brushing
in the open air n ear a sick to simulate a bathroom environment.
Dogs in group 111 were further subdivide into three equal groups
(two dogs per group) for brushing with a target
microorganism-contaminated brush. The group 111 toothbrushes were
initially sterilized and subsequently immersed for 24 hours
containing 106 target microorganisms(B
melaninogenicus, S aureus, or C albicans). The brushing regimen
for all the dogs group 111 was the same as the dogs in groups 1 and
11.
Gingival or other oral lesions were recorded prior the
subsequent day's brushing, with the date and six of then lesions
observed. Each lesion was also cultured. After initial baseline
venous blood cultures, additional venous blood were on dogs from
group 111 within 30 minutes of the first day of the brushing of each
month. These cultures were for both the target microorganism and for
normal oral flora. Additional venous blood cultures were also made
at the discretion of then examiner.
At the ends of the first
phase, six dogs had to be dropped from the study (four for
persistent upper respiratory symptoms and two for difficulty in
handling). After an 18-day normalization period, 18 dogs entered the
second phase of the study. Of the 12 carry-over dogs, those that
were in groups 1 were moved to group 11; those in group 11 were
moved to group 111; and those in group 111 were moved to group 1.
The six new dogs were placed in the appropriate groups so that all
groups had six dogs.
To evaluate the effects for frequent
brushing, all groups in the second phase were brushed on Tuesday,
Wednesday, and Thursday. The second phase also lasted 1 month and,
other than the days of brushing, following the same protocol that
was used in the first phase. After a 12-day normalization period, 18
dogs entered the third phase (all second dogs were used; no new dogs
were added). The group of dogs were again recorded so that each dogs
served as its own control. Twelve dogs had through all three phases
was followed. The brushing protocol of second phase was
followed.
To determine the effects of immunosuppression on ulcer
incidence and blood transmission, two dogs from the group 1 (new
sterile toothbrush), two dogs from group 11 (self-contaminated
toothbrush) and two dogs from group 11(one Candida-brushed
and one Staphylococcus were given 2.5 mg/kg of prednisone
every other day for seven days prior the initiation of the third
phase and every other day for the first 14 days of the third
phase.
Throughout the entire study, the animals were housed under
conditions accredited by the American Association of Accreditation
of Laboratory animal care, The dogs were fed a regular diet and
water libitum. Some dogs required mild sedation, but, with continued
handling, most dogs were easily brushed. The four dogs that
developed respiratory disease in the first phase were successfully
treated, but were replaced prior the second and third phases. Three
litters of healthy puppies were delivered during the time of the
experiments. To maintain uniformity in the brushing, the same
individuals (wearing appropriate protective clothing) brushed all of
the dogs each time. All cultures were processed and evaluated using
the current aerobic, anaerobic, and mycotic techniques. All
toothbrushes were Oral-B No. 35 (Oral-B Laboratories.
Because of
the complexity of the protocol, a four-way analysis of variance was
performed on the data with dogs, drugs, brushing regimen, and nature
of brush as sources of variability. The type 111 sum of squares was
used: Each effect was adjusted for all of the other effects. A
pair-comparison test was carried out with the data from only those
dogs that were brushed with a new sterile toothbrush each time and
those brushed with a self-contaminated toothbrushes in the different
phases, but who were expose to no drugs.
Results
Two hundred nineteen ulcers were recorded in 648 possible
recording for overall cumulative incidence of 0.34 ulcers per dog
per day. The most common sites of ulcers were the attached gingiva
and the vestibule. No difference were noted between acute brushing
and chronic as ulcers occurred throughout each phase.
Fifty-two
ulcers were observed in group 1 animals (sterile toothbrushes); 88
ulcers were observed in group 11 animals (self-contaminated
toothbrushes); and 79 ulcers were notes in groups 111 animals (known
microorganism-contaminated toothbrushes). In addition, gingival and
buccal erythema and buccal mucosal roughness were observed in the
group 111 animals. The total average lesion per dog for all phases
of the study was 2.0 ulcers per dog in group 1, 4.9 ulcers per dog
in group 11, and 4.4 per dog in group 111. If there incidence in
Phase 111 alone is considered, the average lesion per dog in was
3.12 ulcers per dog in group 1, 5.0 ulcers per dog in group 11, and
4.7 ulcers per dog in group 111 for dogs that were not
immunosuppressed. In dogs that were immunosuppressed, there were 5.2
ulcers per dog in group 1, 10.5 ulcers per dog in group 11, and 6.5
ulcers per dog in group 111. If difference in the brushing patterns
are considered, in the first phase of the study (brushing every
other day per week), the average of lesions per dog was 1.7 in group
1, 3.3 in group 11, and 2.8 in group 111. In second phase (brushing
three consecutive days per week), the average number of lesions per
dog was 2.3 in group 1, 4.0 in group 11, and 3.5 in group 111. In
third phase (brushing three consecutive days per week, with some
dogs immunosuppressed). the average number lesions per dog was 5.2
in group 1, 10.5 in group, and 6.5 group 111. Along with an
increased incidence of ulcers, the immunosuppressed dogs from all
three groups had an increased tendency toward gingival bleeding. The
type of known microorganism appeared to make no difference in the
incidence of ulcers: Bacteroides produced the largest number
of ulcers in the first phase; Candida produced the largest
numbers in the second phase; and Staphylococcus produced the
largest number in the their phase. In the third phase (in which both
Candida and Staphylococcus were immunosuppressed), the
dogs exposed to Candida had the lowest incidence of ulcers
and the dogs exposed to Staphylococcus the highest
incidence.
The type of microorganism present intrinsically in the
dog's mouth appeared to effect the results. Dogs that had a range of
microorganisms (normal oral flora) appeared to fewer ulcers than
dogs that had a predominance of Bacteroides. The group of
dogs with the highest incidence of ulcers was the group that had
Bactericides and aerobic enteric microorganisms in
substantial numbers. Similarly, both Bacteriodes and aerobic enteric
microorganisms were often found in the swabs from the individual
ulcers.
Although the incidence was low (four post brushing
positive blood cultures), it appeared that microorganisms can be
transmitted from the oral cavity into the blood in sufficient
numbers that they can retrieved on cultures. One positive culture
was found in both groups 1 and 111, and two positive cultures were
found in group 11.
There appeared to be no consistent pattern of
ulceration as the dogs moved from one group to another. For example,
while dog 2392 had the highest incidence of ulcers when brushed with
its self-contaminated brush in group 11, second phase, it had the
lowest incidence of ulcers in group 1, first phase and group 111,
third phase (even thought it was immunosuppressed in the third
phase). Similarly, dog 1867 (immunosuppressed, group 111,
Staphylococcus contaminated), had on the highest ulcer
incidence in third phase but much lower ulcer incidence in first and
second phases.
Healing appeared to be slow in the
immunosuppressed dogs from all three groups. Healing in other groups
and phases did not appear to have be predicable pattern. For the
most part, all ulcers were healed by the beginning at the next
brushing cycle of a particular phase and often by the next
day.
� Brush type: 0=sterile brush; 1=self-contaminated
brush; 2=contaminted brush.
� Regimen: 0=alternate days of
brushing; 1=consecutive days of brushing.
: Drug: 0=did not
receive drugs; 1= received drug.
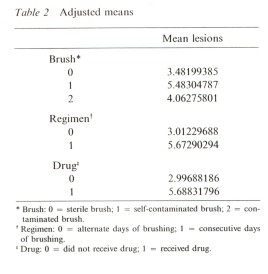
The data used
for the statistical analysis of variance was taken only from 12 dogs
that completed all three phases of the study. Also, due the
differences brought on immunosuppressive drugs, individual sample
sizes were often small. This may account for the fact that, while
the analyses often were near significance, only the brushing regimen
change was found to be statistically significant using the analysis
of variance tests. Table 1 summarize the data from the 12 dogs that
went through all three phases, and Table 2 provided the estimates of
the mean number of lesions by brush, regimen, and drug. The
pair-comparison test confirmed that, regardless of other variables
such as regimen or immunosuppressive drugs, the most oral ulcers
developed in animals in which self-contaminated toothbrushes were
reused; the fewer ulcers developed when a new sterile toothbrush was
used every time. Both statistical tests showed that increasing
brushing significantly increased (P.05) the incidence of oral
ulcers.
discussion
While the clinical observations associated the toothbrush with
(at least) dental disease were important, and while laboratory
observations demonstrated long retention of viable herpes simplex
virus type 1, the results of the present the necessary link to
implicate to toothbrush as a potential transmitter of disease.
12. Further, the findings of the study should cause not
only the dental professional, but also the medical profession, to
consider the influence of the toothbrush on not only the sick
patient but also the "healthy" individual. In light of the evidence,
from the clinical observation to laboratory observation and now in
animal model, it makes sense to recommend that patients with mucosal
disease, periodontal disease, and even dental caries changes their
toothbrushes at regular, short intervals (such as weekly or
biweekly) when they are in active therapy. In the initial study, the
recommendation was made that toothbrushes be changed at least once
per month and at the beginning and end of every illness
1. The recommendation that the toothbrush be stored
outside the moist and contaminated environment of the bathroom is
important. In the dog model, the not only oral flora
(Bateriodes) but also enteric microorganism (such as those
found in moist bathrooms).
From a medical point of view, the
results of the toothbrush studies have a direct application.
Toothbrushes should changed frequency by patients with persistent or
recurrent upper airway and gastrointestinal infections, by patients
who are undergoing bypass surgery or organ/tissue transplantation
(who cannot risk a bacterial/septicemia), and by patients who are
immunocompromised by virtue of diseases such as acquired
immunodeficiency syndrome or chemotherapy for cancer. The authors
have received many anecdotal reports from around the world that
affirm these recommendations since the initial published report and
subsequent publicity. Similarly, preliminary results from a study in
which patient with recurrent herpes labiitis change their
toothbrushes at the beginning of the prodrome, at the end of the
prodrome, or, is vesicle forms, changing their toothbrushes after
the vesicle breaks, indicate a marked decrease in progression from
prodrome to vesicle and from vesicle to multiple vesicles.
While
the present study demonstrated that there was an increase in the
ulcers incidence with increased frequency of brushing, this finding
should not be misconstrued as a rational for not brushing teeth at
all. However, care must be taken with a device (the toothbrush) that
may transmit disease so easily. To refrain from brushing would be to
reverse completely the progress that has been made in preventive
dentistry. The admonition remain: Change toothbrushes frequently.
Design a microbial-resistant toothbrush.
summary
The results of the study indicated that toothbrushing with even a sterile toothbrush produced gingival or mucosal ulceration. Immunosuppersion increased the incidence. Toothbrushing with a self-contaminated brush had the highest incidence of the any groups tested. Further, the incidence was magnified by immunosuppression. Brushing with known microorganisims inceased the incidence of ulcerations as compared to the use of a sterile toothbrush; however, it was not as harmful as brushing with a self-contaminted brush. The ulcerations did not consistently contain the known or target microorgamism. Although the incidence was low, there was evidence to suggest possible transmission of microorganisms from the ulcer into the blood. Daily brushing increased the incidence of ulcerations. The healing of the ulcerations appeared to be dependent on the brushing process and was slowed by the reintroduction of microorganisms. Immunospression increased by the incidence of ulcerations. Most healing occured within one day with reintroduction of microorganisms.
Featured Articles
Read MoreCustomer Testimonials
-
- "Purebrush provides the protection they need..."
- "Because people forget to change their toothbrushes as often as they should, Purebrush provides the protection they need."
-
- "Dr visits have decreased dramatically..."
- Purebrush is wonderful! I have two small children and our doctor visits have decreased dramatically since we purchased our Purebrush. I really think your product is great and I believe that you are doing a great thing for people's health.
Read More




